Periarthritis of the shoulder, commonly known as frozen shoulder, can feel like a never-ending struggle. The stiffness, pain, and limited range of motion can interfere with even the simplest tasks, like reaching for a cup or putting on your coat. But you’re not alone—this condition affects millions of people, especially those over the age of 40. The good news? There are effective treatments available to help you regain your shoulder’s mobility and reduce discomfort.
In this blog, we’ll explore what periarthritis is, why it happens, and how you can treat it to get back to living your life with full shoulder function.
Jump To:
TLDR – Quick Guide
- What is periarthritis (frozen shoulder)? It’s a condition that causes stiffness and pain in the shoulder joint due to inflammation and thickening of the capsule surrounding the shoulder.
- What causes periarthritis? The exact cause is often unknown, but it can result from prolonged shoulder immobility, injury, or surgery.
- What are the treatment options? Treatment includes physical therapy, pain management (NSAIDs or injections), and in some cases, surgery.
- Can it be prevented? Early mobilization after an injury or surgery and regular shoulder exercises can reduce the risk of developing periarthritis.
Detailed Breakdown: Understanding and Treating Periarthritis
1. What Is Periarthritis (Frozen Shoulder)?
Periarthritis, or frozen shoulder, is a condition characterized by stiffness, pain, and restricted movement in the shoulder joint. This happens because the connective tissue surrounding the shoulder (the capsule) becomes inflamed and thickened, restricting motion. The progression of periarthritis typically follows three stages:
- Freezing Stage: Shoulder movement becomes increasingly painful, and range of motion is limited.
- Frozen Stage: The pain may lessen, but stiffness remains, making it difficult to move the shoulder.
- Thawing Stage: Gradually, the shoulder begins to loosen, and range of motion improves.
The entire cycle of frozen shoulder can last anywhere from several months to up to two years if left untreated.
2. Common Causes of Periarthritis
While the exact cause of periarthritis is often unclear, several factors are linked to its development, including:
- Prolonged Shoulder Immobilization: This could result from recovering from surgery or an injury that leads to limited use of the shoulder.
- Injury or Surgery: Trauma to the shoulder or post-operative recovery can trigger the condition.
- Age and Gender: People aged 40 and older, particularly women, are more likely to develop frozen shoulder.
- Medical Conditions: Diabetes, thyroid disorders, and cardiovascular diseases have been associated with an increased risk of developing periarthritis.
Understanding the risk factors can help guide prevention and treatment strategies.
3. Effective Treatment Options for Periarthritis
Treatment for periarthritis typically depends on the stage of the condition and the severity of symptoms. Here are the most common approaches to managing the condition:
- Physical Therapy: The cornerstone of periarthritis treatment is physical therapy. Stretching and mobility exercises help maintain and gradually increase range of motion. A physical therapist can create a customized exercise plan based on your needs, focusing on the frozen shoulder’s current stage.
- Pain Relief with Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen or aspirin, can help reduce pain and inflammation. For more severe pain, your doctor may recommend corticosteroid injections, which can offer temporary relief and improve shoulder mobility.
- Manual Therapy: Techniques such as joint mobilization and massage, often performed by a physical therapist or chiropractor, can help loosen the shoulder capsule and alleviate stiffness.
- Hydrodilatation: This minimally invasive procedure involves injecting fluid into the shoulder joint to expand the capsule, helping improve range of motion and reduce pain.
- Surgical Treatment: In rare cases, if other treatments don’t provide relief, surgery (such as shoulder arthroscopy) may be recommended to remove adhesions and scar tissue from the shoulder capsule. Most people respond well to non-surgical treatments, but surgery is an option for long-lasting cases of frozen shoulder.
4. Preventing Periarthritis
While not all cases of frozen shoulder can be prevented, there are steps you can take to reduce your risk:
- Early Mobilization: After an injury or surgery, it’s important to gently start moving your shoulder as soon as possible (following your doctor’s advice). Prolonged immobility is a key risk factor for periarthritis.
- Regular Shoulder Exercises: Stretching and strengthening exercises can help maintain your shoulder’s flexibility and range of motion.
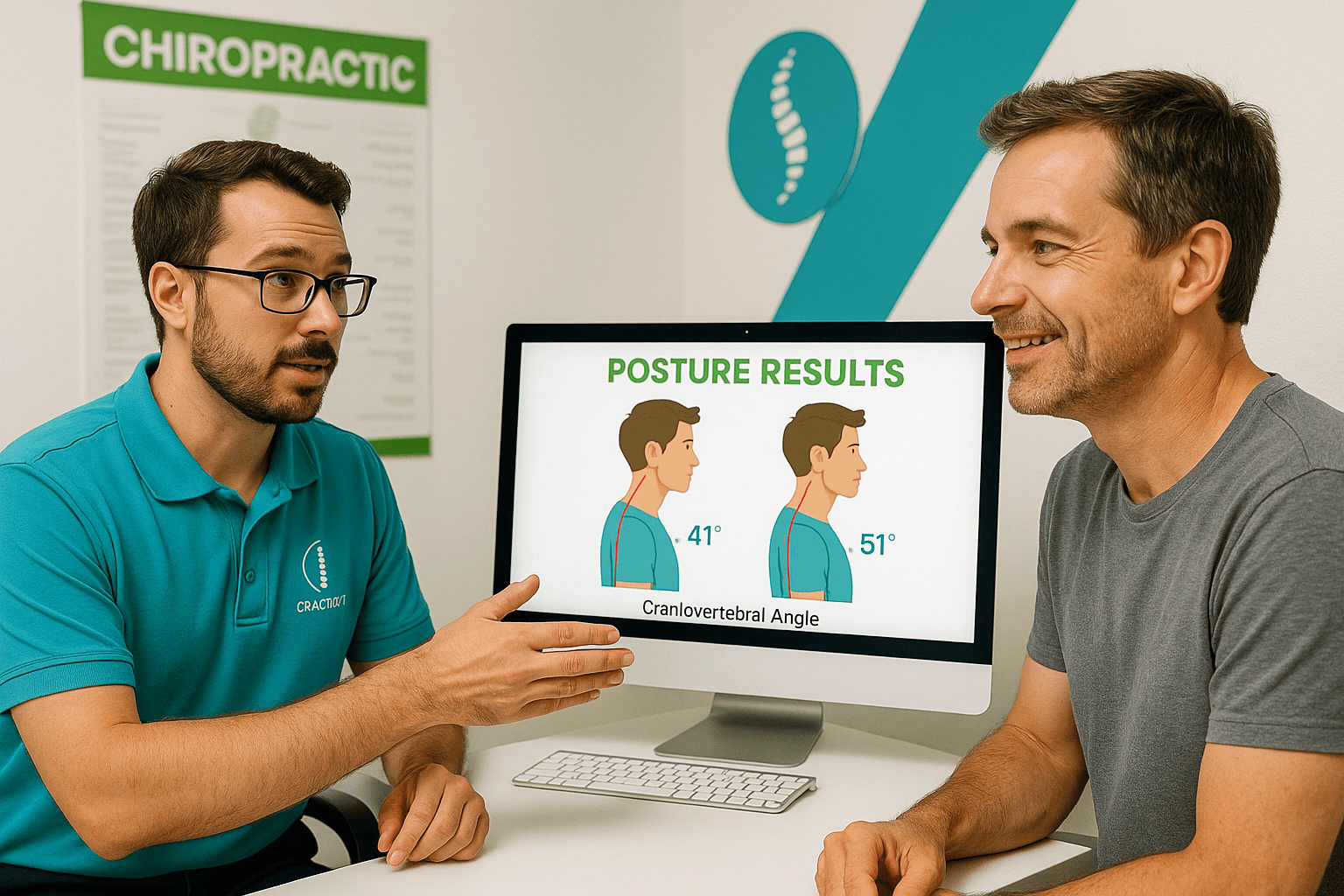
- Good Posture: Poor posture, especially while sitting at a desk or slouching, can strain your shoulders and lead to conditions that may promote stiffness.
Key Takeaways
- Periarthritis, or frozen shoulder, is a painful condition that can severely limit shoulder mobility.
- Treatment options range from physical therapy and pain relief to minimally invasive procedures like hydrodilatation, with surgery as a last resort.
- Early mobilization and regular shoulder exercises are key to preventing periarthritis, especially after an injury or surgery.
- With proper treatment, most people recover from frozen shoulder without the need for surgery.
Shoulder pain and stiffness can seriously affect your day-to-day life, but there are plenty of treatment options available to help you regain control. Whether you’re in the early stages of periarthritis or have been struggling with limited shoulder mobility for months, a combination of therapy and proper management can help ease the discomfort and get you back to normal.
FAQs
1. How long does periarthritis (frozen shoulder) take to heal?
Periarthritis can take anywhere from 6 months to 2 years to resolve, depending on the severity and treatment. With proper management, symptoms often improve much faster, but the full recovery process can be lengthy. Physical therapy can significantly speed up recovery.
2. Is frozen shoulder more common in women than men?
Yes, frozen shoulder is more common in women, particularly those between the ages of 40 and 60. Hormonal changes, such as those during menopause, are thought to play a role in increasing the risk for periarthritis.
3. Does frozen shoulder always require surgery?
No, most cases of frozen shoulder can be successfully treated without surgery. Physical therapy, medications, and other non-invasive treatments are usually effective. Surgery is typically only considered for severe cases that don’t respond to conservative treatments.
4. Can frozen shoulder recur after treatment?
While frozen shoulder usually doesn’t recur in the same shoulder after treatment, some people may develop it in the opposite shoulder. Maintaining shoulder mobility and regular exercise can help lower the risk of recurrence.
5. What’s the difference between frozen shoulder and rotator cuff injury?
Frozen shoulder involves stiffness and a limited range of motion caused by inflammation of the shoulder capsule, while rotator cuff injuries typically involve damage to the tendons or muscles around the shoulder. The two conditions can cause similar symptoms, but they require different treatments.